Postural orthostatic tachycardia syndrome (POTS) is a blood circulation disorder that affects the autonomic nervous system and manifests in an abnormal increase in heart rate upon standing up. Understanding the various signs and symptoms can lead to earlier diagnosis and expert treatment to manage debilitating effects.
What Is POTS?
POTS is caused by faulty autonomic regulation resulting in an exaggerated heart rate increment of 30+ beats per minute (or exceeding 120 bpm) when moving from lying down to an upright position that is sustained.
This leads to noticeable symptoms within 10 minutes of standing as circulatory abnormalities limit normal blood flow.
What Are The Signs And Symptoms Of Pots?
Common POTS symptoms upon standing include:
| Signs | Symptoms |
|---|---|
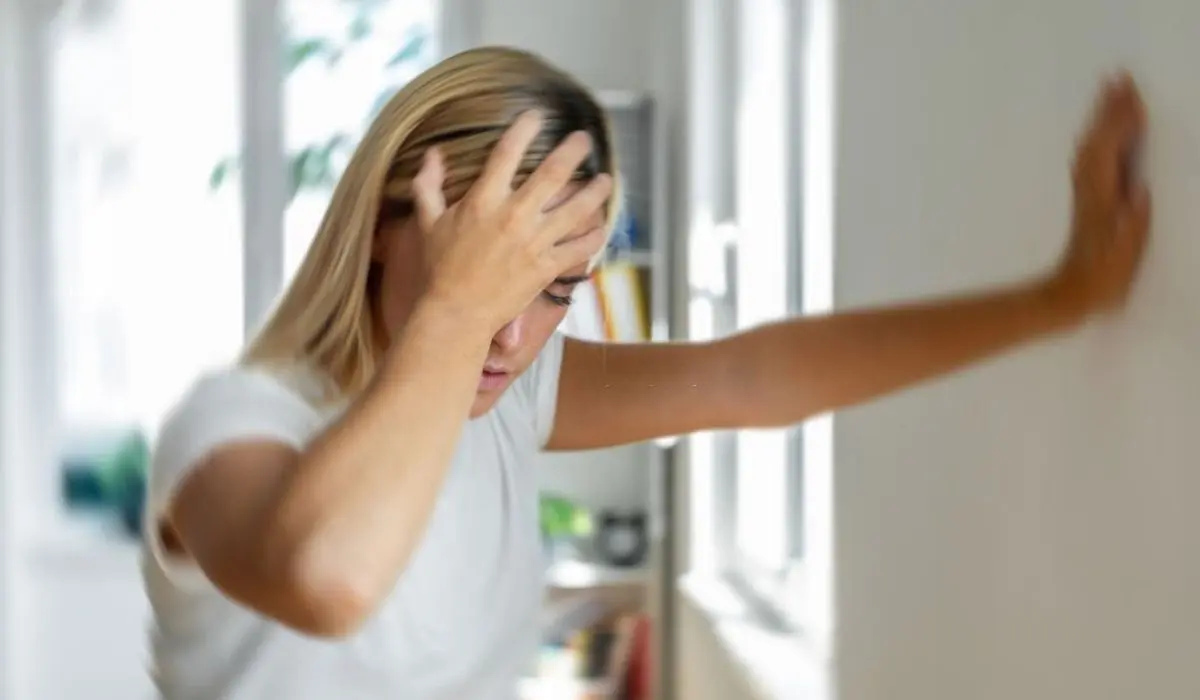
| Lightheadedness, dizziness, or vertigo | Sudden head rush or fainting |
| Fatigue and weaknes | Exhaustion, exercise intolerance |
| Fatigue and weakness | Unsafe unsteady feeling |
| Vision changes | Blurry vision, spots, tunneling |
| Headache | Pulsing migraine-like headaches |
| Stomach problem | Nausea, bloating, pain, diarrhea |
| Flushing or pallor | Sudden skin redness or paleness. |
| Sweating | Increased bursts of perspiration throughout the day. |
| Insomnia | Disrupted sleep cycles. |
How Are POTS Diagnosed?
Diagnosis involves:
🔹 Patient history – Chronic and recurring upright symptoms for more than6 months.
🔹 Tilt-table test – Measures heart rate and blood pressure response to positional change.
🔹 Active stand test – Documents 30+ bpm increase within 10 minutes of standing.
🔹 Ruling out other causes – Anemia, dehydration, medications causing tachycardia.
Diagnostic criteria require sustained tachycardia upon standing with notable symptoms but no signs of orthostatic hypotension greater than 20 mm Hg systolic drop.
What Are The Causes Of Pots?
POTS frequently arises due to:
🔹 Autoimmune response – Antibodies blocking receptors impairing vascular function.
🔹 Neuropathic origins – Small fiber peripheral neuropathy disrupting blood flow.
🔹 Deconditioning – Prolonged inactivity from illness causing blood volume decline.
🔹 Genetic factors – Gene polymorphisms affecting blood pressure and heart rate control.
Often no definitive cause is found but these factors play a contributory role. Viral illness, pregnancy, injury, or trauma can trigger the onset of POTS.
What Are The Risk Factors For Pots?
🔹 Gender – 5 times more prevalent in females, potentially hormonal link.
🔹 Age – Most commonly affects women under age 50.
🔹 Joint hypermobility – More elastic connective tissue and veins.
🔹 Low blood volume – Reduced fluids and sodium.
🔹 Sedentary lifestyle – Prolonged time spent sitting or lying down.
🔹 Prior viral infection – Links to onset 1-3 months post-viral illness.
How Is POTS Treated?
POTS has no cure but symptom management approaches include:
🔹 Increasing fluid and salt intake – Improves blood volume.
🔹 Compression garments – Prevent blood pooling in extremities.
🔹 Exercise training – Strengthens muscles pumping blood back to the heart.
🔹 Raising the head of the bed – Gravity shift minimizes nighttime tachycardia.
🔹 Avoiding triggers – Heat, alcohol, and big meals affect circulation.
🔹 Medications – Beta blockers slow heart rate; fludrocortisone ups blood volume.
🔹 Physical therapy – Strengthening and reconditioning.
What Are The Complications Of POTS?
If not properly managed, POTS can lead to:
➜ Presyncope and fainting – resulting in injury.
➜ Dehydration and salt depletion from frequent urination and sweating.
➜ Poor physical conditioning – Muscle weakening from reduced activity.
➜ Obesity – Due to exercise limitations and fatigue.
➜ Depression and anxiety – From chronic illness.
➜ Social isolation – Due to flares from exertion.
Can POTS Be Prevented?
There are no definitive ways to prevent POTS but staying active, maintaining a healthy weight, consuming salt and fluids, and promptly treating potential triggering events like viruses may lower risk.
POTS often goes undiagnosed so recognizing symptoms early aids diagnosis and treatment to reduce severity.
Conclusion
POTS significantly disrupts autonomic nervous system regulation but expert treatment can help restore stable circulatory function and manage symptoms.
Educating those at risk allows prompt diagnosis and support. With consistent lifestyle adjustments and therapy, quality of life markedly improves and flare severity lessens.
FAQs
Yes, POTS can substantially impair daily function meeting ADA disability criteria if symptoms are severe.
Symptoms may fluctuate in severity but require ongoing management. Some patients experience periods of remission
While not directly life-threatening, injury from fainting poses risks. Proper treatment and prevention reduce complications.
In some cases, POTS arising after pregnancy, trauma or a virus will resolve after 6-24 months. But most require ongoing treatment.
Lifestyle adjustments like fluid intake, compression garments, and reconditioning exercise plus medication if needed.

