Diabetic Charcot foot, also known as Charcot neuroarthropathy, could be an extreme complication of diabetes that can lead to noteworthy foot deformations and inability in cases cleared out untreated. But can it be switched? In this article, we’ll investigate the nature of Charcot Foot, its causes, indications, and accessible treatment alternatives to address this challenging condition. We’ll also dig into the significance of early diagnosis and prevention to help people with diabetes avoid the onset of Charcot’s foot.
Diabetic Charcot Foot: All You Need To Know
Diabetic Charcot foot may be a dynamic, degenerative condition that influences the bones and joints within the feet of people with diabetes. It ordinarily arises due to nerve harm, a condition known as fringe neuropathy, which disables sensation and proprioception (the sense of one’s body position) within the feet. This neuropathy can lead to unnoticed wounds and breaks within the foot, which, when left untreated, can result in deformations and joint instability.
Causes and risk factors
Several components contribute to the improvement of Charcot’s foot:
Diabetes: The foremost common fundamental condition is diabetes, especially when ineffectively managed, leading to high blood sugar levels and nerve damage.
Peripheral Neuropathy: Nerve harm, regularly caused by uncontrolled diabetes, diminishes the capacity to feel pain or inconvenience within the feet, making people less mindful of injuries.
Trauma: A severe injury, such as strolling on a foot with a push brake, can trigger the onset of Charcot’s foot.
Poor Blood Stream: A decreased bloodstream to the limits can moderate the body’s common recuperating processes.
Hereditary Components: There may be a hereditary inclination that makes a few people more helpless to Charcot’s foot.
Symptoms
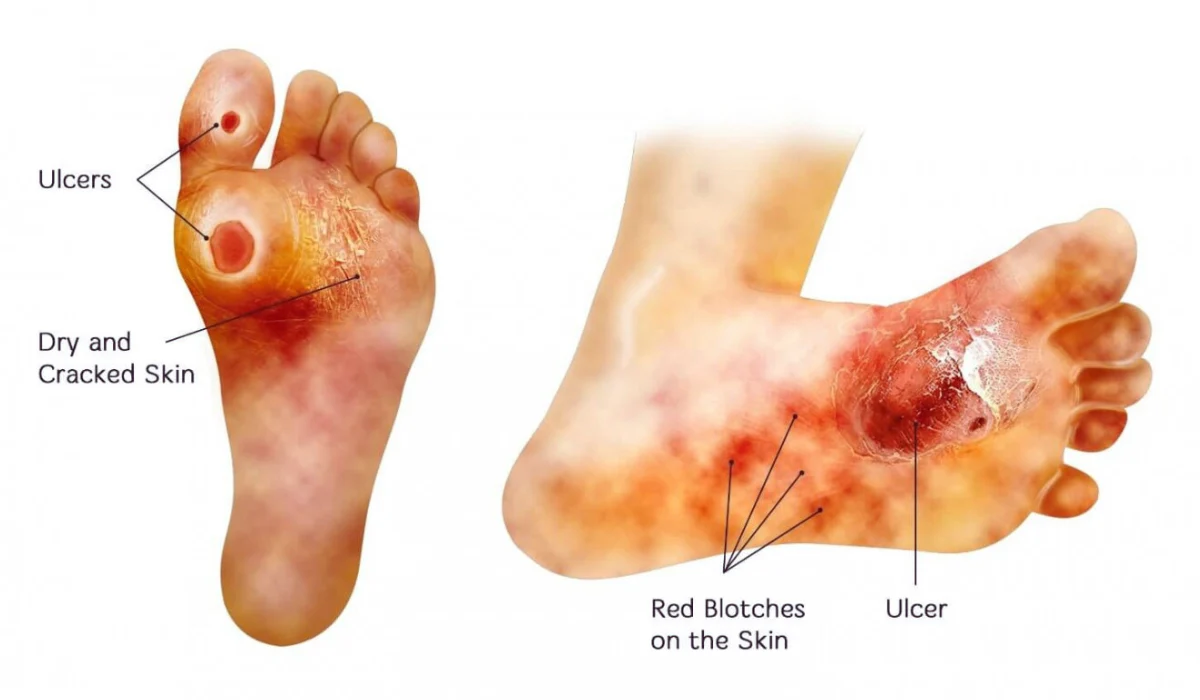
The initial indications of Charcot’s foot can be unpretentious, counting swelling, warmth, and redness within the affected foot. As the condition advances, the following indications may become evident:
◾Deformities: The curve of the foot may collapse, leading to an irregular shape
◾Instability: Influenced people may have difficulty walking due to joint instability.
◾Ulcers: Open bruises or ulcers can form on the foot, which can be challenging to mend due to decreased blood flow.
◾Infection: In serious cases, contamination can happen and may indeed lead to removal if not treated promptly.
◾Chronic Pain: Charcot foot can cause tireless torment within the influenced foot, making day-to-day exercises challenging.
Treatment Options
Charcot foot could be a complex condition that requires a multi-faceted approach to administration. Whereas it may be challenging to “switch” the condition totally, the essential objectives of treatment are to:
✅ Immobilization: Rest and immobilization are fundamental to preventing harm. Non-weight-bearing casts or braces may be utilized. Immobilization can shift in terms depending on the seriousness of the condition.
✅ Offloading: Specialized footwear or custom orthotics can help disperse weight more equally and decrease weight in influenced ranges. Offloading gadgets is significant for avoiding assist harm and permitting the foot to heal.
✅ Surgical Intercession: In a few cases, surgery may be vital to redress serious deformities or address complications like contaminations or ulcers. Surgery can include realignment of bones and joint stabilization.
✅ Glycemic Control: Overseeing diabetes and keeping blood sugar levels within target ranges is significant in avoiding advanced nerve harm and complications. Tight glycemic control can moderate the movement of the Charcot’s foot.
✅ Rehabilitation: Physical treatment can help patients regain quality, adjustability, and versatility in their affected feet. Workouts and stride preparation are basic components of rehabilitation.
✅ Wound Care: For people with ulcers or contamination, meticulous wound care is crucial. This may incorporate cleaning, dressings, and anti-microbial, if necessary.
✅ Orthopedic Footwear: Custom orthopedic footwear can provide included support and offer assistance to avoid injury.
✅ Patient Education: Education about approximately legitimate foot care, diabetes management, and the significance of standard check-ups is fundamental for anticipating complications.
Prevention and early diagnosis
Preventing Charcot’s foot is basic, as early conclusion and mediation can enormously progress outcomes. Here are a few preventive measures for people with diabetes:

▪ Regular Foot Exams: People with diabetes ought to have normal foot exams to screen for any signs of neuropathy or Charcot’s foot. Early detection is key.
▪ Foot Care: Day-by-day foot care, including counting, checking for bruises or injuries, washing and drying the feet, and keeping the toenails trimmed, is essential.
▪ Proper Footwear: Wearing well-fitting, steady shoes and maintaining a strategic distance from strolling unshod can diminish the risk of injury.
▪ Glycemic Control: Keeping up great blood sugar control is foremost. Routinely checking blood glucose levels and taking them after a diabetes administration can help anticipate neuropathy.
▪ Smoking cessation: Smoking can disable circulation and increase the chance of complications. Quitting smoking is exceedingly beneficial.
Conclusion
While it may not be possible to switch to diabetic Charcot foot, early determination, and comprehensive treatment can altogether move forward the condition and offer assistance to patients to keep up useful, pain-free feet. It is fundamental for people with diabetes to be proactive in overseeing their condition and look for restorative attention if they suspect any foot-related issues. With appropriate care and the direction of healthcare experts, people with Charcot’s foot can improve their quality of life and diminish the risk of genuine complications. Avoidance and early intervention are significant in tending to this challenging condition and protecting the versatility and well-being of those influenced by diabetes. If you or a loved one has diabetes, keep in mind that great foot care is an indispensable important portion of general diabetes administration, and early activity can make a critical distinction within the result of Charcot’s foot.
FAQ
Q1: What exactly is diabetic Charcot foot?
A1: Diabetic Charcot foot is a serious condition that affects the feet of individuals with diabetes. It’s a bit like a structural problem in the foot that can happen when you have diabetes. The bones and joints in the foot get affected, making it difficult to walk.
Q2: Is Charcot foot curable?
A2: Do not forget that though it will be hard to eradicate Charcot Foot in most cases, once it has been detected and well taken care of, it will prove to be a significant advantage. It’s all about handling it and ensuring that other problems do not arise from it.
Q3: Why do people suffer from Charcot’s foot?
A3: The major causes include diabetes and what is known as ‘peripheral neuropathy’—an interferer with the ability to know you have stepped on something using one’s feet. There are other factors, such as injuries and poor circulation of blood, and sometimes it also runs in the family.
Q4: How do I know if I might have Charcot’s foot? What should I look out for?
A4: Initially, the symptoms include a swollen foot, a warm foot, or a reddish foot. As things worsen, your foot may change its shape, it might give way, giving you open sores and infected wounds, or you may experience constant foot pain indefinitely.

