Polycystic ovary syndrome (PCOS) is a common hormone disorder affecting up to 10% of women. While PCOS has classic signs, researchers now recognize various subtypes that each respond best to tailored treatments. Understanding the different PCOS presentations can help guide appropriate management.
What Is PCOS?
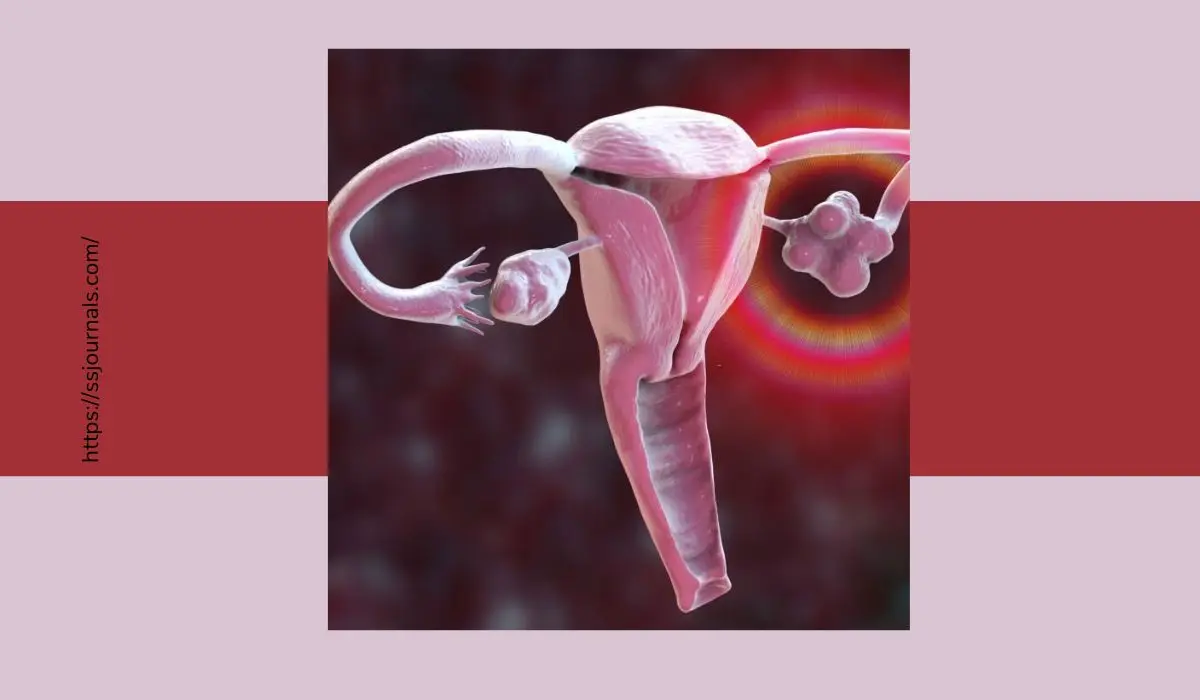
PCOS involves hormone imbalances that disrupt ovulation and create symptoms like irregular periods, excess hair growth, and sometimes infertility. Cysts on the ovaries are common as well. The exact causes are unknown but include insulin resistance, genetics, and environmental factors.

There are several PCOS variants that have slightly different symptoms:
4 Types Of PCOS
Insulin Resistant PCOS
This is the most common type affecting around 50-70% of women with PCOS. As the name suggests, insulin resistance is the major feature. Weight gain, darkening skin patches, skin tags, and acanthosis nigricans (dark, velvety patches on the skin) are common physical findings. These women have an increased risk of developing diabetes and cardiovascular problems.
Inflammatory PCOS
This type accounts for about 25% of PCOS cases. It is associated with high levels of inflammatory markers like CRP and IL-6 as well as increased white blood cells in the follicular fluid.
Women have more dramatic PCOS symptoms like severe acne, alopecia (excess hair loss), and scalp hair loss. They tend to have normal body weight.
Adrenal PCOS
About 15% of women have this type, characterized by excess adrenal androgens. Women show symptoms of high testosterone – severe acne, alopecia, hirsutism – but have normal insulin levels. Polycystic ovaries may not be present.
Ovulatory PCOS
A small percentage (10-15%) of women continue having ovulatory cycles but have hyperandrogenism and polycystic ovarian morphology. They don’t show typical symptoms of PCOS like irregular periods but may have acne, scalp hair loss, or unexplained infertility.
Related: How To Treat Hormonal Imbalance In Teenage Girls? Risk Factors!
Causes Of PCOS
While the exact causes are unknown, factors contributing to PCOS development include:
➜ Genetics – family history raises risk
➜ Insulin resistance
➜ High androgen levels
➜ Environmental toxins
➜ Obesity
➜ Stress
➜ Sedentary lifestyle
Treatment Of PCOS
Treatments target managing symptoms and reducing long-term risks:
➜ Birth control pills to regulate menstrual cycles
➜ Metformin and lifestyle changes to improve insulin sensitivity
➜ Anti-androgens like spironolactone to reduce excess hair
➜ Weight loss for overweight women
➜ Acne treatments
➜ Fertility medications if trying to conceive
Conclusion
Identifying your specific PCOS subtype allows for more customized and effective treatment approaches tailored to your particular hormone profile and symptoms. Work with your doctor to determine the right management plan.
FAQs
Yes, though less common some relatively lean women get diagnosed with hormonal PCOS without weight being the primary driver.
Yes, having a mother or sister with PCOS significantly raises your risk. Certain genes and variants are linked to susceptibility.
Extended-cycle pills with low androgen progestins like drospirenone, desogestrel, or norethindrone work well for classic high-androgen PCOS.
While first-line for classic PCOS, metformin may be less effective for variants like inflammatory PCOS with different drivers.
Weight loss can help manage symptoms but lower weight alone doesn’t necessarily reverse the root hormonal and metabolic imbalances driving PCOS.
More: What Is The Role Of Estrogen And Progesterone In Menstrual Cycle?