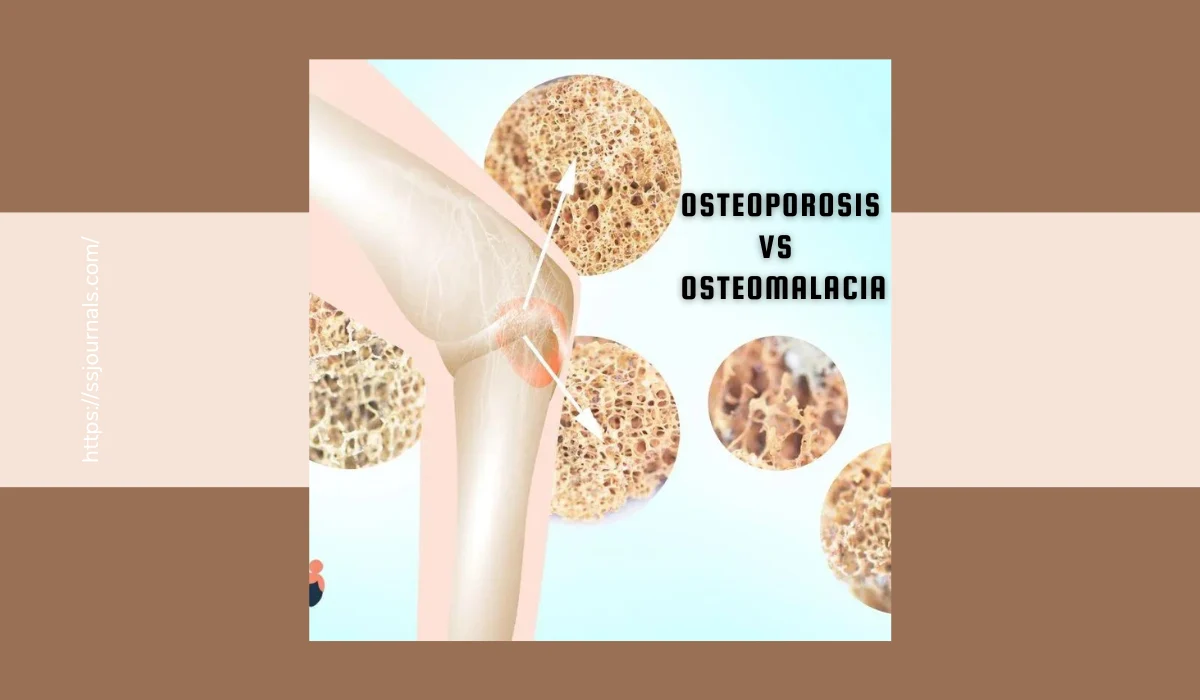
Bone health is significant for our general well-being. Among the different bone-related conditions, osteoporosis and osteomalacia are two regularly misconstrued conditions. Whereas their names sound to some degree alike, they particularly disagree with interesting characteristics, causes, indications, and medications. In this comprehensive article, we’ll investigate osteoporosis and osteomalacia in profundity, giving you a comprehensive understanding of these bone infections and how to distinguish between them.
Osteoporosis – The Quiet Danger to Bone Health
Osteoporosis is frequently referred to as the “quiet illness” since it advances stealthily, without displaying discernible indications until a break happens. It essentially influences older people, with postmenopausal ladies being especially powerless. Let’s dig into the specifics of osteoporosis:
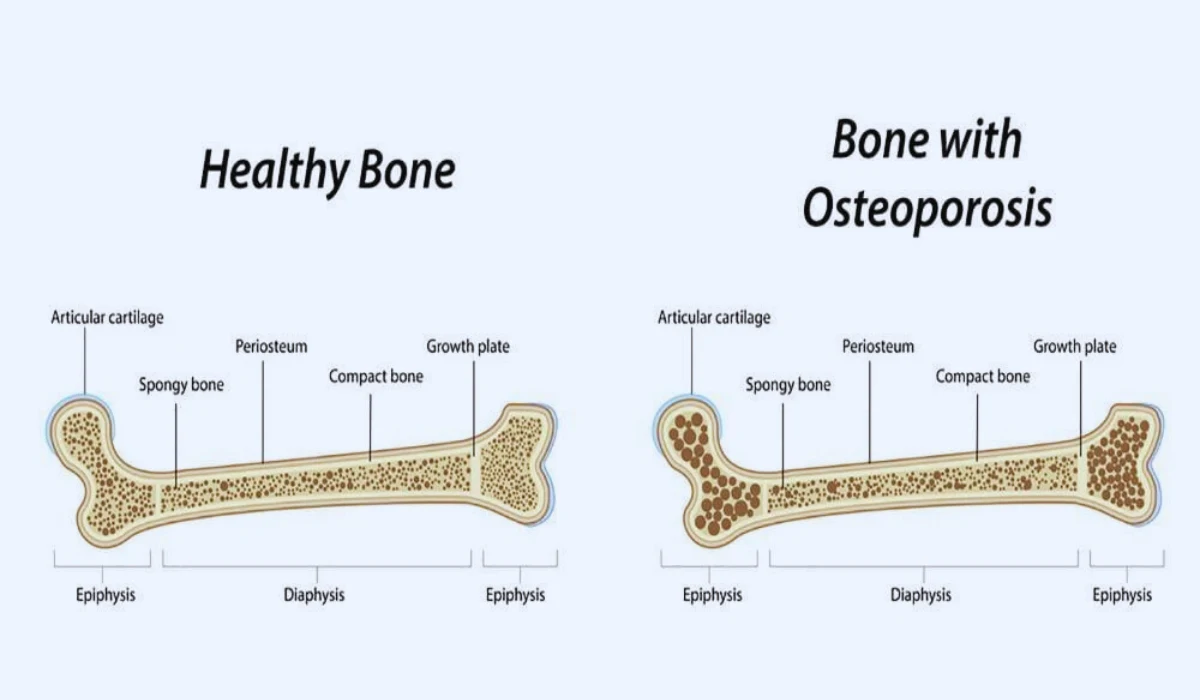
🔶 Bone Density Loss: Osteoporosis is characterized by the continuous loss of bone thickness. Over time, bones end up permeable and lose their structural integrity. This debilitating bone thickness is the trademark of osteoporosis.
🔶 Fracture Chance: Individuals with osteoporosis are at an essentially higher risk of breaks, especially within the hip, spine, and wrist. What’s especially concerning is that these breaks can happen with negligible injury or indeed during ordinary exercises. A straightforward drop or a wheeze can lead to a break in somebody with osteoporosis.
🔶 Common Causes: The most common causes of osteoporosis are hormonal changes, especially the reduction of estrogen amid menopause. Estrogen plays a crucial part in keeping up bone thickness, and its decrease leads to an expanded chance of osteoporosis. Other risk factors include maturing, family history, low body weight, and certain solutions, such as corticosteroids.
🔶 Silent Disease: Osteoporosis is frequently called a “silent disease” since it advances without recognizable side effects until a break happens. Tragically, by the time a break happens, noteworthy bone thickness misfortune has as of now occurred.
🔶 Prevention and Treatment: Preventive measures for osteoporosis include keeping up an adjusted count of calories rich in calcium and vitamin D, locking in weight-bearing works, and, in a few cases, taking medicine. Early determination through bone thickness tests is vital for successful administration. These tests offer assistance to healthcare experts in evaluating bone thickness and distinguishing people at risk of osteoporosis.
Osteomalacia – Softening of the Bones
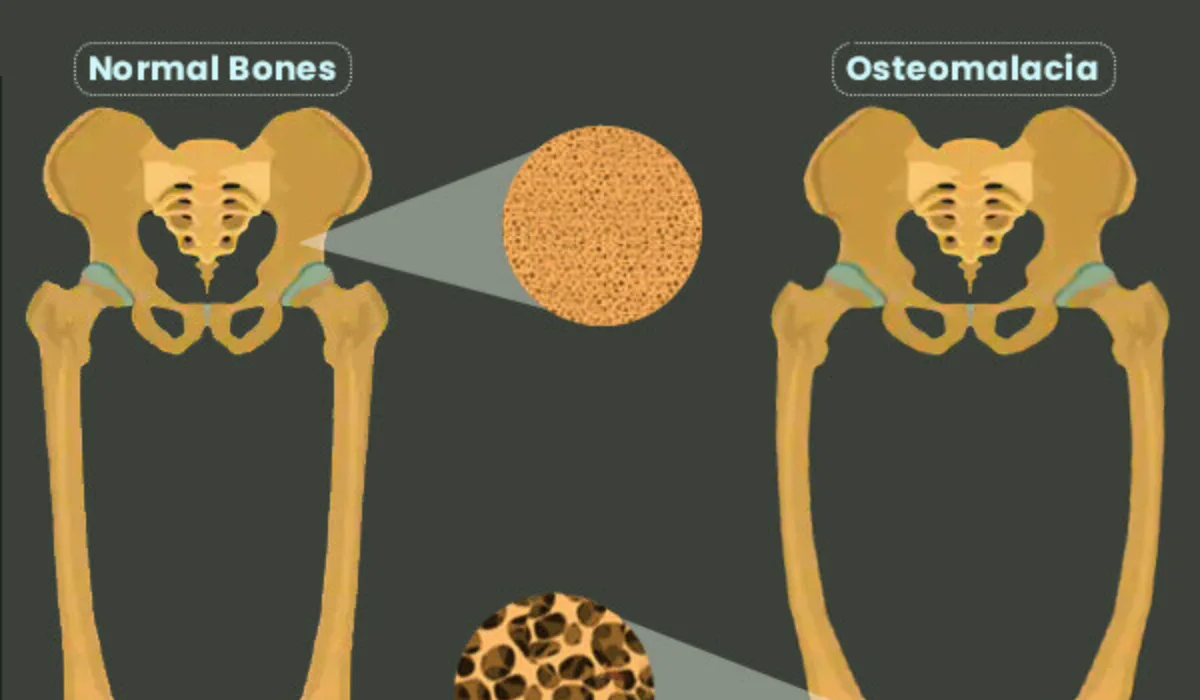
Osteomalacia, a condition characterized by softening of the bones, is unmistakable from osteoporosis. It can influence people of all ages, and its essential cause could be a lack of fundamental minerals like vitamin D, calcium, and phosphate. Let’s investigate the interesting characteristics of osteomalacia:
◼ Mineral Insufficiency: The root cause of osteomalacia is ordinarily an insufficiency in fundamental minerals, especially vitamin D, calcium, and phosphate. These minerals are pivotal for legitimate bone mineralization.
◼ Muscle Weakness and Pain: Not at all like osteoporosis, osteomalacia frequently presents with muscle shortcomings, bone pain, and delicacy. These side effects can make day-by-day exercises challenging and lead to a decay in by and large physical health.
◼ Disabled Mineralization: Osteomalacia happens when the bone matrix is inadequately mineralized, coming about in frail bones that can twist or distort beneath weight. This softening of bones may be an unmistakable highlight of osteomalacia.
◼ Secondary Causes: Other than nutritional lacks, osteomalacia can also be caused by certain restorative conditions, such as kidney infection or malabsorption. These conditions can meddle with the body’s capacity to assimilate and utilize fundamental minerals.
◼ Treatment: The essential approach to treating osteomalacia includes tending to the basic dietary insufficiencies. This can be regularly accomplished through supplementation of vitamin D, calcium, or phosphate, and nearby dietary alterations. Distinguishing and tending to the basic causes, such as kidney malady or malabsorption clutters, is additionally vital in managing osteomalacia.
Distinguishing Between Osteoporosis and Osteomalacia
Distinguishing between osteoporosis and osteomalacia is pivotal for precise conclusions and suitable treatment. Healthcare professionals depend on restorative history, physical exams, and symptomatic tests to distinguish between the two conditions. Here are a few of the common strategies utilized for this purpose:
🔹 Bone Density Tests: Bone thickness filters, such as Dual-Energy X-ray Absorptiometry (DEXA) filters, are commonly utilized to survey bone thickness and analyze osteoporosis. These tests can offer assistance in deciding the quality and thickness of bones.
🔹 Blood Tests: Blood tests may be performed to degree levels of particular minerals and hormones, such as calcium, vitamin D, and parathyroid hormone (PTH). Unusual levels of these substances can give experiences into the basic causes of bone disorders.
🔹 X-rays: X-rays are regularly utilized to imagine bones and assess their auxiliary astuteness. In cases of osteoporosis, X-rays may uncover signs of bone misfortune and breaks. Be that as it may, X-rays are less compelling in diagnosing osteomalacia, as the softening of bones may not be as apparent on X-ray images.
🔹 Medical History: A nitty gritty restorative history can give important data about hazard components and side effects, making a difference in healthcare experts making a precise determination. It’s critical to share any important data about family history, past breaks, or therapeutic conditions that will be contributing to the bone disorder.
Prevention and Management
Preventing and overseeing both osteoporosis and osteomalacia is fundamental for keeping up bone well-being and general well-being. Here are a few techniques and approaches for avoidance and management:
Preventing Osteoporosis:
Count calories: An adjusted slim-down wealth in calcium and vitamin D is basic for keeping up bone well-being. Nourishments like dairy products, leafy greens, and braced cereals can contribute to satisfactory calcium intake.
✅ Exercise: Locks in weight-bearing exercises, such as walking, running, and strength training, can offer assistance in constructing and keeping up bone density.
✅ Medicine: In some cases, healthcare experts may prescribe medicines like bisphosphonates or hormone substitution treatment to anticipate and assist bone misfortune in people at high risk.
Managing Osteoporosis:
Pharmaceutical: For people diagnosed with osteoporosis, medication may be endorsed to strengthen bones and reduce the risk of breaks. Common medications include bisphosphonates, denosumab, and teriparatide.
Way of life Changes: Way of life adjustments, and counting drop avoidance techniques, can diminish the hazard of breaks in people with osteoporosis.
FREQUENTLY ASKED QUESTIONS
Q1: What is the most important distinction between osteoporosis and osteomalacia?
Osteoporosis is characterized by a continuous misfortune of bone thickness, driving to fragile and permeable bones, essentially influencing more seasoned people. Osteomalacia, on the other hand, is the softening of bones due to a lack of fundamental minerals, frequently coming about in muscle shortcomings and bone pain.
Q2: What are the common side effects of osteoporosis?
Osteoporosis is frequently alluded to as a “noiseless malady” since it advances without recognizable side effects until a break happens. Common indications incorporate an increased risk of breaks within the hip, spine, and wrist. Breaks can happen with negligible injury or amid ordinary activities.
Q3: How do I know in case I have osteomalacia?
Osteomalacia ordinarily presents with indications such as muscle shortcoming, bone torment, and delicacy. If you’re encountering these side effects, it’s fundamental to”>to allude to a healthcare proficient who can perform demonstrative tests to affirm the diagnosis.
Q4: Can osteoporosis happen in more youthful individuals?
While osteoporosis is more common in more seasoned people, it can influence more youthful individuals, especially if they have particular chance components, such as hormonal lopsided characteristics or drawn-out utilization of drugs that contribute to bone loss.
Q5: How are osteoporosis and osteomalacia diagnosed?
Both conditions can be analyzed through a combination of strategies, counting restorative history, physical exams, blood tests to evaluate mineral and hormone levels, bone thickness looks (like DEXA filters), and X-rays to imagine bone wellbeing.