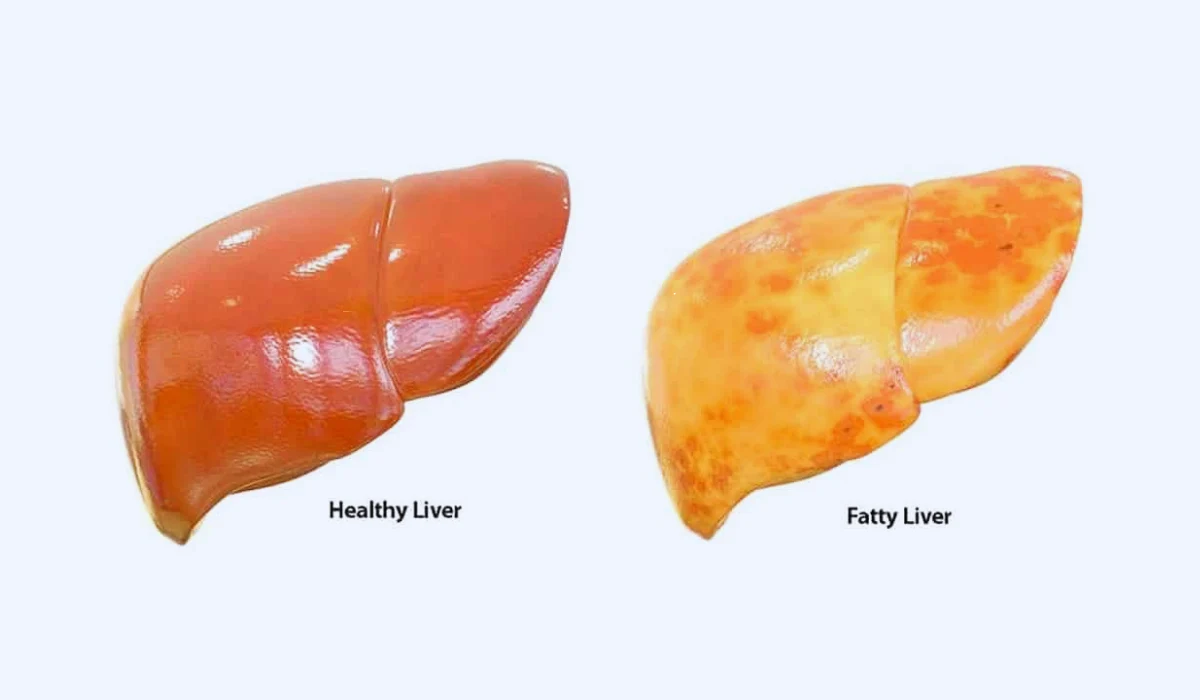
Hepatic steatosis refers to a popular but frequently undiagnosed abnormal state in which there is too much fat within the liver cells. Although a fatty liver does not necessarily show severe signs, it could result in even worse consequences, such as liver cirrhosis or cancer, if ignored. This article explores the symptoms, causes, and treatment options of fatty liver, as it is one of the most underrated illnesses in the world despite affecting thousands of people.
Fatty Liver: Symptoms
Fatty liver symptoms can change, and in a few cases, people may not notice any noticeable signs. In any case, when indications do show, they may include:
🔸 Fatigue: A common complaint among people with fatty livers is persistent weariness and shortness of breath. The liver, an imperative organ for vitality and metabolism, may struggle to operate ideally when influenced by excess fat. Weariness can essentially affect daily exercise and quality of life.
🔸 Abdominal Discomfort: Pain or inconvenience within the upper right side of the guts can
happen due to liver inflammation or broadening. This indication is often gentle but ought to not be disregarded because it may show progressing liver harm that requires attention.
🔸 Swelling: A fatty liver can lead to fluid maintenance, resulting in swelling within the abdomen and legs. This is often characteristic of more advanced liver harm and warrants restorative consideration. Swelling can contribute to distress and may be related to other complications.
🔸 Jaundice: In severe cases, the liver’s failure to handle bilirubin may lead to jaundice, characterized by yellowing of the skin and eyes. Jaundice could be a clear sign of impeded liver function and may be accompanied by dark-colored pee and pale-colored stools.
🔸 Weight Loss: Unexplained weight misfortune may be related to progressed stages of fatty liver disease, signaling critical liver brokenness. Weight misfortune can be unintentional and may result from a combination of factors, including a decreased craving and a modified metabolism.
Fatty Liver: Causes
Understanding the causes of fatty liver disease is pivotal for anticipation and administration. Common contributing factors include:
Poor Diet: Eating less saturated fats, sugars, and refined carbohydrates advances the collection of fat within the liver. Usually frequently seen in people who eat less processed foods. Making dietary changes may be a key step in avoiding and managing liver disease.
Obesity: Excess body weight, especially stomach corpulence, could be a critical hazard for a fatty liver. The liver may battle to prepare and metabolize fat viably within the vicinity of corpulence. Accomplishing and maintaining a healthy weight is imperative for liver health.
Type 2 Diabetes: Insulin resistance, a trademark of type 2 diabetes, plays a significant role in the advancement of a fatty liver. Elevated insulin levels contribute to expanded fat capacity within the liver. Appropriate diabetes administration, counting medicine, and lifestyle changes are basic for controlling fatty liver.
High Cholesterol: Elevated levels of cholesterol and triglycerides within the blood can contribute to the buildup of fat within the liver. This is often regularly related to being slim and tall in unfortunate fat. Dietary adjustments and cholesterol-lowering medicines may be suggested to address this factor.
Alcohol Consumption: Over-the-top liquor admissions may be a well-known cause of alcoholic fatty liver disease. Inveterate liquor mishandling can lead to aggravation and fat amassing within the liver cells. Total liquor forbearance is significant for ending the progression of alcoholic fatty liver disease.
Treatment
Addressing fatty liver includes a multifaceted approach pointed at way-of-life adjustments, dietary changes, and, in a few cases, restorative intercession. Here are the key components of a comprehensive treatment plan:
✅ Lifestyle Changes:
Adopting a solid way of life is vital. A customary workout, at least 150 minutes per week, can help with weight administration and move forward in affectability. Physical action isn’t as advantageous for the liver but it is for general cardiovascular health.
Smoking cessation is fundamental, as smoking contributes to irritation and oxidative stress, which burden the liver. Stopping smoking can emphatically affect liver function and diminish the chance of complications. Adequate sleep is pivotal for general well-being, including liver function. Point to 7-9 hours of quality rest each night to bolster the body’s natural healing processes.
✅ Dietary Modifications:
Limit the admission of immersed fats, sugars, and prepared nourishments. In step, center on a count of calories rich in natural products, vegetables, whole grains, and incline proteins. A well-balanced and nutritious count of calories is essential for giving the liver the nutrients it needs to work optimally. Consider the Mediterranean or Sprint Slim Down, both of which emphasize heart-healthy nourishment and have appeared to have benefits for liver wellbeing. These diets are rich in cancer prevention agents, anti-inflammatory compounds, and omega-3 fatty acids.
✅ Weight Management:
Achieving and keeping up a solid weight is paramount in overseeing a fatty liver. Indeed, an unassuming weight misfortune of 5–10% can lead to noteworthy enhancements in liver function. interview with an enlisted dietitian can give personalized direction for weight management.
✅ Medications:
In a few cases, healthcare experts may endorse solutions to control fundamental conditions such as diabetes and high cholesterol. These medicines point to contributing factors to fatty liver and may be a significant component of the, by and large, treatment plan.
✅ Alcohol Abstinence:
For people with alcoholic-fatty liver disease, complete abstinence from liquor is non-negotiable. Typically, this is the most effective way to prevent further liver harm and advance recuperation. Bolster bunches and counseling can be profitable assets for individuals striving to maintain liquor abstinence.
✅ Regular Monitoring:
Individuals diagnosed with fatty liver ought to experience standard check-ups to screen liver function and address any rising concerns promptly. This incorporates scheduled blood tests to evaluate liver proteins and imaging studies, such as ultrasound or MRI, to assess the degree of liver fat. Customary observing is basic for following advance and altering the treatment plan as needed.
Conclusion:
Fatty liver may be a reversible condition, especially when recognized and tended to in its early stages. By making positive life changes, people can not only oversee the side effects but also move forward the overall well-being of their liver. A discussion with a healthcare professional is vital for an accurate determination and personalized treatment plan.
Understanding the link between way of life factors and fatty liver encourages people to take control of their well-being and anticipate the movement of this common liver condition. Whereas it is frequently related to weight and destitute dietary choices, it can influence individuals of all body sorts. Subsequently, cultivating mindfulness about the side effects, causes, and treatment alternatives for fatty liver is essential for advancing liver well-being and anticipating long-term complications. If you suspect you may have a fatty liver or are at risk, look for direction from a healthcare professional to set out on a path toward a more advantageous liver and overall well-being.
FAQ
Q1: What precisely is fatty liver, and how does it influence me?
Fatty liver, or hepatic steatosis, is when your liver amasses excess fat. This condition can shift from gentle to extreme and may lead to aggravation and liver harm if it is not addressed.
Q2: What signs ought I seek to distinguish fatty liver?
Common signs include feeling determinedly tired, distress within the upper right side of your midriff, swelling in your guts and legs, yellowing of the skin and eyes (jaundice), and unexplained weight loss.
Q3: What causes fatty liver, and am I at risk?
Poor calorie count, weight, type 2 diabetes, high cholesterol, and over-the-top liquor utilization are common causes. Anybody, in any case of body sort, can create a fatty liver, even though components like hereditary qualities and certain therapeutic conditions can contribute.
Q4: How is fatty liver analyzed, and what should I expect?
Diagnosis regularly includes imaging, like ultrasound or MRI, and blood tests to evaluate liver function. Now and then, a liver biopsy may be prescribed for a more in-depth evaluation.
Q5: Are there particular diets that can offer assistance with fatty liver, and how do I make changes?
Yes, a count of calories in saturated fats, sugars, and processed foods, combined with an emphasis on natural products, vegetables, whole grains, and inclined proteins, is suggested. Consider the Mediterranean or sprint slim down, counsel with a dietitian for personalized advice