Joint injuries and degenerative joint diseases like osteoarthritis can be extremely debilitating and difficult to treat. In recent years, there has been growing research interest in using peptides – short chains of amino acids – to potentially regenerate cartilage, reduce inflammation, and aid joint repair.
Proponents suggest peptides may provide a safer, less invasive alternative to joint replacement surgery in some cases. However, more rigorous study is still needed to fully understand the viability of peptides for widespread use in repairing joints. This article explores the current evidence behind joint-healing peptides. top 8 healing peptides, How Do Peptides Work for Injury Recovery and Repair? And so on.
What Are Peptides and How Might They Help Joints?

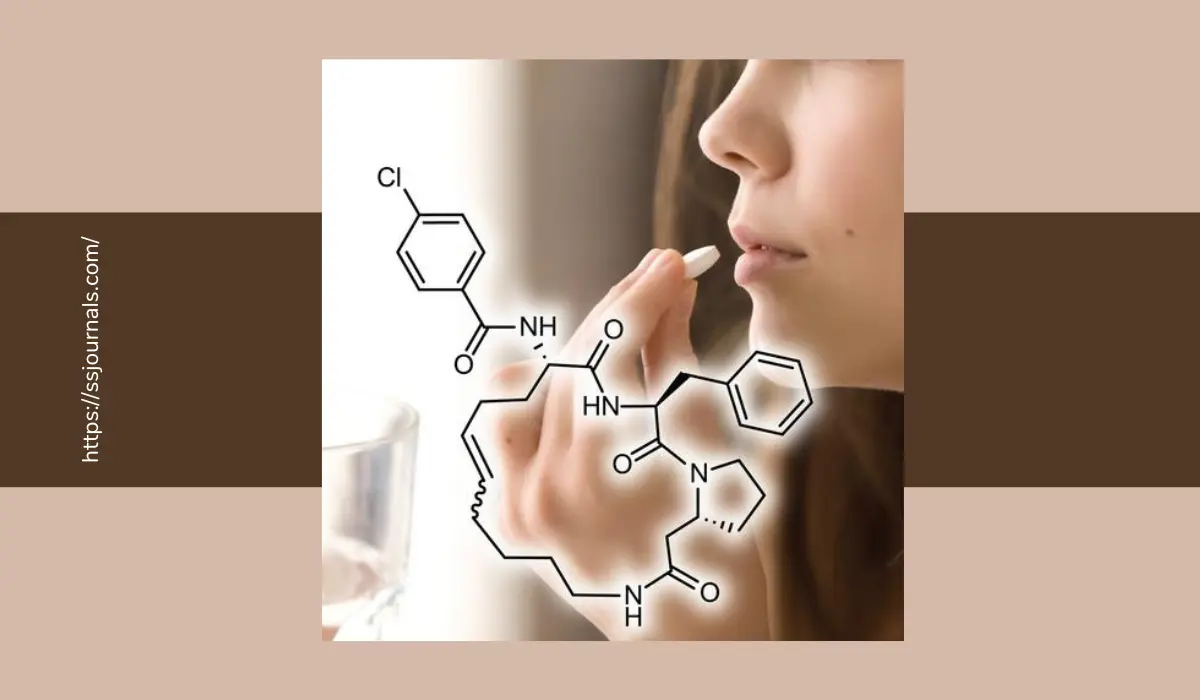
Peptides are compounds containing two or more amino acids linked together in a chain. Several natural peptides play important roles in regulating bodily processes related to inflammation and tissue repair. Synthetic peptide supplements attempt to harness these effects to improve recovery. Some prime examples include:
- TB-500: A synthetic version of a naturally occurring peptide found in thymosin beta proteins. Animal studies show that TB-500 may reduce inflammation, increase cell growth, and speed wound healing.
- BPC-157: Derived from protective peptides made in the gut. Research indicates that BPC-157 might help heal damaged and inflamed tendons, muscles, ligaments, and cartilage.
- Ipamorelin: A growth hormone peptide that may stimulate cartilage development and enhance joint lubrication.
- CJC-1295: Works synergistically with sermorelin as an analog GHRH to substantially elevate growth hormone and metabolism to aid fat loss.
- Melanotan II: A synthetic peptide hormone that stimulates melanin production, leading to increased pigmentation and photoprotection; it has been investigated for sunless tanning and enhancing libido.
- Thymosin Beta 4: By reducing inflammation and promoting soft tissue healing, Thymosin Beta-4 shows promise for treating tendon, ligament, and even cartilage injuries when injected directly into the joint.
- MGF: As a growth factor capable of activating local stem cells and boosting protein synthesis, MGF could potentially support the regeneration of cartilage and connective tissues if delivered to injured joints.
- IGF-1: IGF-1 plays a key role in cartilage development and stimulating chondrocyte proliferation for natural joint repair processes, suggesting therapeutic IGF-1 administration could assist joint injury healing and inhibit osteoarthritic cartilage breakdown.
The exact mechanisms behind these peptides’ joint regenerating potential require further elucidation. However, they appear to modulate inflammation, support the formation of collagen scaffolding, and recruit stem cells involved in tissue regeneration.
Peptides For Joint Repair: Understanding The Benefits And Risks
Multiple preclinical and small human trials demonstrate the tantalizing benefits of using peptides to treat joint problems:
Accelerating Recovery From Sports Injuries
In injured athletes with knee ligament tears and tendon damage, BPC-157 injections appeared to quickly restore range of motion and enable a faster return to training. The peptide outperformed standard rehab protocols in these preliminary cases.
Potential Cartilage Regeneration
Rodent osteoarthritis models treated with BPC-157 showed almost complete cartilage regeneration in affected joints – even in advanced disease stages. This may point to peptides’ capacity not just to reduce inflammation but actually to repair joint structure.
Synergistic Effects of Stem Cell Therapy
Pairing peptides like TB-500 with intraarticular stem cell injections shows particular promise. In multiple reports, this combination enabled even severely inflamed joints with significant cartilage loss to return to normal function and movement.
Additionally, the peptide CJC-1295 works synergistically with sermorelin as an analog GHRH to substantially elevate growth hormone and metabolism to aid fat loss. This may complement stem cell-based regeneration.
Relief of Chronic Joint Pain
An uncontrolled case series on meloxicam combined with certain “healing peptides” achieved substantial reductions in knee osteoarthritis symptoms – including 50% and greater improvements in joint pain, stiffness, and function. These striking early findings warrant controlled follow-up.
While not definitive, these studies lay the groundwork for larger-scale trials to clarify peptides’ clinical utility in treating common joint disorders.
Potential Benefits of Peptide Joint Therapy
If borne out in additional rigorous trials, key advantages of peptide-based joint regeneration may include:
- Less Invasive Treatment – Unlike joint replacements or cell transplants requiring surgery, peptides could simply be injected.
- Superior Safety Profile – With shorter amino acid chains, peptides tend to demonstrate better tolerability and fewer side effects than larger protein medications.
- Disease Modifying Effects – Peptides may facilitate lasting structural repairs rather than just reducing inflammation.
- Enhanced Healing Environment – Peptides’ tissue regenerating properties may complement surgical/cell procedures improving outcomes.
- Wide Applicability – Peptide therapy could assist recovery from sports injuries and benefit chronic degenerative diseases like osteoarthritis.
The benefits of healing peptides for bodybuilding
Healing peptides like BPC-157, TB-500, IGF-1, and Thymosin Beta 4 have gained attention in bodybuilding circles for their potential to accelerate injury recovery and aid muscle growth. When injected directly into damaged muscle tissues, these peptides may reduce inflammation, support regenerative processes, and enhance protein synthesis.
Although formal research is still lacking, anecdotal experiences among bodybuilders suggest peptide therapies could allow faster return to training after strains or tears, while also possibly improving hypertrophy from workouts when combined with proper resistance exercise protocols.
However, effects likely vary based on factors like nutrition, genetics, and the bodybuilder’s overall steroid/drug regimen. More controlled trials are needed to truly gauge if reported benefits outweigh possible long-term health risks.
Risks and Unknowns Demanding Further Study
Despite encouraging early peptide research for joint repair, important efficacy and safety questions remain unresolved:
- Optimal Protocols Uncertain – More comparisons of dosing strategies, peptide combinations, and delivery methods are imperative.
- Lack of Large Scale Trials – Small early trials offer clues but definitive confirmation demands multi-center studies with more patients.
- Long-Term Effects Not Established – Would repairs from temporary peptide treatment last or might unforeseen complications emerge later?
- Impact on Disease Progression Unclear – Even if peptides reduce joint pain would they slow the advance of degenerative conditions?
- Regulatory Status Still Developing – As “supplements” many peptides occupy gray areas requiring greater oversight as their pharmaceutical use grows.
While joint-healing peptides sit tantalizingly close to clinical utility, realizing their full potential requires methodical science to establish firm foundations guiding medical application.
Conclusion
In the constant battle against joint injuries and relentless diseases like osteoarthritis, peptide-based regeneration approaches hold genuine promise as less invasive alternatives to major surgery. Exciting preclinical and early human data establish proof-of-principle for peptides’ capacity to dampen inflammation and foster lasting tissue repairs.
However, sizable trials definitively demonstrating efficacy and safety remain lacking at this still exploratory stage. A much more rigorous study on optimal treatment protocols and potential long-term effects stands mandatory before peptide therapies can achieve standard roles alongside mainstay options like physiotherapy, steroid injections, or joint replacement. While peptides may never fully substitute for these approaches in advanced disease, they do offer alluring possibilities – perhaps restoring joints early in degeneration or improving outcomes when combined with cell therapies or surgery.
For joints facing inevitable doom absent new solutions, healing peptides should command robust investigation to assess if they might help stall or even reverse seemingly inexorable damage in at least some portion of patients. Guarded optimism grounded in emerging science offers a balanced perspective, avoiding unfounded hype and recognizing peptides’ legitimate promise of restoring joint health.